Could the Brain's Mast Cells Be Causing Chronic Fatigue Syndrome (ME/CFS)?
"We propose that stimulation of hypothalamic mast cells by environmental neuroimmune pathogenic and stress triggers activates microglia leading to focal inflammation in the brain and disturbed homeostasis." Theoharides et. al., 2018
Dr. Theoharis Theoharides is an MD and PhD who has published almost 400 papers. A pioneer in the field of mast cell research, Theoharides runs the mastcellmaster.com website and has produced a line of dietary supplements to tamp down mast cell activity. Just a couple of days ago he led an NIH sponsored workshop "Mast Cell Triggers and Mediators Beyond Allergy and Tryptase". Recently he took up the subject of chronic fatigue syndrome (ME/CFS), energy metabolism and mast cell activation in a paper "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome-Metabolic Disease or Disturbed Homeostasis?First Theoharides examines the idea that problems with energy metabolism are causing ME/CFS. He agrees that the energy problems ME/CFS patients experience are due to problems with energy depletion, stating that, "Much evidence suggests that the pathophysiology of ME/CFS is highly associated with alterations in normal energy metabolic processes and abnormalities in cellular bioenergetics", but then spoils it a bit by suggesting that deconditioning could be the cause.Similarly, in his section on metabolic syndrome and ME/CFS, Theoharides proposes that problems with blood pressure regulation and insulin resistance, "most probably reflect the lack of physical activity and prolonged lack of muscle use in ME/CFS patients". But then Theoharides agrees that a hypometabolic state which reduces energy production (ATP) is probably present. He also agrees that the typical ME/CFS phenotype, i.e. the way the disease presents itself clinically, largely matches that found in people with mitochondrial diseases. He notes that muscle biopsies do show signs of mitochondrial problems.On the other hand, people with ME/CFS don't have the mitochondrial DNA mutations, enzyme issues or drops in ATP production typically found in those diseases.He suggests that free radicals produced by pro-inflammatory cytokines could be whacking the mitochondria in ME/CFS so hard so as to blunt their ATP production, but then notes that no consistent evidence of cytokine upregulation, has been found.After basically concluding that energy production is a problem in ME/CFS but that none of the usual suspects are the likely answer, and citing the fact that physical, mental and/or emotional stress tends to do people with ME/CFS in, Theoharides, like the Cortene group, turned to the HPA axis.Many ME/CFS studies, after all, have found problems in the HPA axis - one of the two stress response systems in our bodies - and the axis does affect metabolism. Could it be ground zero for ME/CFS?
But then Theoharides agrees that a hypometabolic state which reduces energy production (ATP) is probably present. He also agrees that the typical ME/CFS phenotype, i.e. the way the disease presents itself clinically, largely matches that found in people with mitochondrial diseases. He notes that muscle biopsies do show signs of mitochondrial problems.On the other hand, people with ME/CFS don't have the mitochondrial DNA mutations, enzyme issues or drops in ATP production typically found in those diseases.He suggests that free radicals produced by pro-inflammatory cytokines could be whacking the mitochondria in ME/CFS so hard so as to blunt their ATP production, but then notes that no consistent evidence of cytokine upregulation, has been found.After basically concluding that energy production is a problem in ME/CFS but that none of the usual suspects are the likely answer, and citing the fact that physical, mental and/or emotional stress tends to do people with ME/CFS in, Theoharides, like the Cortene group, turned to the HPA axis.Many ME/CFS studies, after all, have found problems in the HPA axis - one of the two stress response systems in our bodies - and the axis does affect metabolism. Could it be ground zero for ME/CFS?
Mast Cell Activation
Theoharides thinks so. He proposes that mast cell activation, smack dab in the heart of the HPA axis - the hypothalamus - is occurring in ME/CFS.If mast cells are involved in ME/CFS it wouldn't be that much of a surprise. They are, after all, extraordinarily versatile immune cells which have the capability to produce the extraordinary number of symptoms found in ME/CFS. Containing hundreds of immune mediators, they can respond to a wide range of stimuli - from pathogens (including mold) to hormones to toxins to immune and neuronal factors.Best known as mediators of allergic reactions, they're also "sensors of environmental and psychological stress." These "sensors" can secrete localized "danger signals" which stimulate the microglia in small pockets of the body/brain. Theoharides proposes that a mast-cell induced inflammation in the hypothalamus could be causing chronic fatigue syndrome (ME/CFS).
The Mast Cell / Hypothalamus Inflammation Connection
Several studies suggest that inflammation is present in the brains of people with ME/CFS and/or fibromyalgia and Theoharides thinks he knows how this occurs.It turns out that most of the brain’s histamine is located in the hypothalamus. Plus mast cells are also found in the pituitary gland (as well as the thyroid, the thalamus and the pineal gland).Theoharides’ mast cell ME/CFS hypothesis begins with a hormone - corticotropin releasing hormone (CRH) - which is released by the hypothalamus during stress and which has been implicated in a series of neuroinflammatory disorders.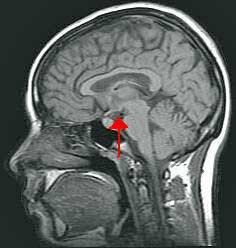 Theoharides believes CRH stimulates the mast cells in the hypothalamus (and elsewhere) to produce something called vascular endothelial growth factor (VEGF), which then increases the permeability of the blood-brain barrier (BBB). That leaky BBB then allows more immune cell (e.g. mast cell) and perhaps pathogen infiltration into the brain and bingo, you have inflammation.Once in the hypothalamus those activated mast cells produce more CRH, further tweaking the hypothalamus and producing compounds such as histamine, tryptase and mtDNA which send the microglia into a frenzy, causing them to release inflammatory cytokines/chemokines (IL-1B, IL-6, CCL2) that further disrupt hypothalamic functioning.While the pro-inflammatory cytokines are busy doing that, Theoharides also believes they're likely whacking the mitochondria in the brain and body, causing centrally (brain induced) as well as peripherally produced (body induced) fatigue, sleep problems, etc.The main problem, though, is a not an overt threat but hyper-sensitized microglial cells pouring out inflammatory factors in response to the slightest stressors.(Meanwhile, mast cell activation in the pineal, pituitary and thyroid glands may also be disturbing sleep and producing more fatigue.)And there you have it. Mast cells - which just happen to be concentrated in several of the brain areas implicated in ME/CFS - have gone off the rails. They're causing microglial cells to produce pro-inflammatory factors which are producing inflammation in key parts of the brain that are involved in the stress response, fatigue, sleep, etc.
Theoharides believes CRH stimulates the mast cells in the hypothalamus (and elsewhere) to produce something called vascular endothelial growth factor (VEGF), which then increases the permeability of the blood-brain barrier (BBB). That leaky BBB then allows more immune cell (e.g. mast cell) and perhaps pathogen infiltration into the brain and bingo, you have inflammation.Once in the hypothalamus those activated mast cells produce more CRH, further tweaking the hypothalamus and producing compounds such as histamine, tryptase and mtDNA which send the microglia into a frenzy, causing them to release inflammatory cytokines/chemokines (IL-1B, IL-6, CCL2) that further disrupt hypothalamic functioning.While the pro-inflammatory cytokines are busy doing that, Theoharides also believes they're likely whacking the mitochondria in the brain and body, causing centrally (brain induced) as well as peripherally produced (body induced) fatigue, sleep problems, etc.The main problem, though, is a not an overt threat but hyper-sensitized microglial cells pouring out inflammatory factors in response to the slightest stressors.(Meanwhile, mast cell activation in the pineal, pituitary and thyroid glands may also be disturbing sleep and producing more fatigue.)And there you have it. Mast cells - which just happen to be concentrated in several of the brain areas implicated in ME/CFS - have gone off the rails. They're causing microglial cells to produce pro-inflammatory factors which are producing inflammation in key parts of the brain that are involved in the stress response, fatigue, sleep, etc.
The Hypothalamus - A Central Player
A couple of years ago, though, Dr. Bateman of the Bateman-Horne Center came to a similar conclusion: she believes that inflammation in the lower part of the brain containing the thalamus, hypothalamus and pituitary plays a key role in ME/CFS. The hypothalamus, which sits just above the brain stem, regulates blood pressure, temperature, and hormone and water content.Dr. Bateman noted that these organs control the hormones (the hypothalamus is the hormonal control center of the brain) and much of the autonomic nervous system, and then pointed out a long list of hormonal problems (corticotrophin releasing hormone (CRH), growth hormone, thyroid, LH/FSH, vasopressin, oxytocin) that have been uncovered in ME/CFS and fibromyalgia.She believes that a "limbic encephalitis" is causing a cascade of problems going both ways; up into the cortex and down into the thalamus, pituitary and the autonomic nervous system.https://www.healthrising.org/blog/2014/07/17/mystery-longer-big-picture-emerging-chronic-fatigue-syndrome-dr-bateman-talks/
Treatment
Theoharides blasted through several possible mitochondrial enhancing treatments (bezafibrate, angiotensin II inhibitors, CoQ10, Losartan) which he didn't find all that much promise in, before focusing on magnesium, which he noted plays a "critical role in energy metabolism and in maintaining normal muscle function(ing)".Theoharides cited studies indicating that magnesium supplements are able to significantly increase muscle strength and endurance and did so, interestingly enough, by enhancing glucose availability in the brain (possibly low in ME/CFS) and muscles, and by delaying and/or reducing lactate accumulations (possibly high in some people with ME/CFS/FM).Then it was on to flavonoids, which Theoharides reported have anti-inflammatory, anti-oxidant and neuroprotective effects. Genistein can reduce muscle fatigue while epigallocatechin, naringin and curcumin have been shown to ameliorate ME/CFS symptoms in experimental models. Astragalus flavonoids, olive extract, and quercetin may have similar effects.Luteolin was the highlight of the bunch. With its mast cell inhibiting, anti-oxidant, anti-inflammatory, microglia inhibitory and neuroprotective properties, luteolin is very high on Theoharides’ list, and in 2015 he produced a paper extolling its benefits. (One study found that tetramethoxyluteolin or methlut appears to be the most effective mast cell inhibiting form of luteolin and is more effective than cromolyn.) Theoharides cited studies that luteolin improved symptoms in autism spectrum disorder (ASD), post-Lyme Syndrome and brain fog in (the not particularly rigorous) open-label trials.Theoharides has hailed fatigue and mast cell inhibiting properties of flavonoids before and has even produced his own line of supplements, but his statement that, "novel treatment approaches are required to address the central pathogenic processes" in these diseases indicates that, in their current form, these flavonoids are not the answer.One of the problems has been that it’s hard to get these substances into the brain. At the end of the paper, though, Theoharides proposes a different way of supplement administration that may be more effective.
Intranasal Administration
"Intranasal administration of select flavonoids may reduce inflammation in the hypothalamus and correct the central pathogenesis of ME/CFS."
Intranasal administration - basically a shot of volatilized factors into the nose and hopefully eventually into the hypothalamus- is getting more and more attention. Theoharides even suggested if it worked it could even correct the problem. No studies have been done, but since the hypothalamus sits behind the amygdala, which is right behind the nose, it's possible intranasal supplementation could help dampen down inflammation there.Flavonoids are just the beginning of the intranasal administration story, though. Over the last couple of years more and more people with ME/CFS/FM have been experimenting with intranasal administration of insulin and glutathione.Plus, Theoharides mentioned another intranasal option -microvesicle trapped curcumin – that is emerging. Curcumin is perhaps the most scintillating of all the natural anti-inflammatories, but bioavailability has been a challenge.In 2015 Theoharides proposed that intranasal administration of tetramethoxyluteolin might be useful as well.A blog on intranasal administration is coming up.
No studies have been done, but since the hypothalamus sits behind the amygdala, which is right behind the nose, it's possible intranasal supplementation could help dampen down inflammation there.Flavonoids are just the beginning of the intranasal administration story, though. Over the last couple of years more and more people with ME/CFS/FM have been experimenting with intranasal administration of insulin and glutathione.Plus, Theoharides mentioned another intranasal option -microvesicle trapped curcumin – that is emerging. Curcumin is perhaps the most scintillating of all the natural anti-inflammatories, but bioavailability has been a challenge.In 2015 Theoharides proposed that intranasal administration of tetramethoxyluteolin might be useful as well.A blog on intranasal administration is coming up.
Conclusion
Dr. Theoharides agrees that problems with energy metabolism are likely present in ME/CFS but proposes that their genesis probably lies in mast cell activation in the hypothalamus and other brain organs. Theorharides suggests that corticotropin releasing hormone produced by the hypothalamus activates masts cells to produce substances that activate the microglia, causing the production of pro-inflammatory substances which produce centrally or brain induced fatigue and autonomic nervous system issues. Mast cell activation in the pituitary and thyroid produces further problems with sleep, fatigue and cognition.Theorharides also proposes that intranasal application of anti-inflammatory substances such as cucurmin and luteolin may be able to access the hypothalamus thus tamping down the neuroinflammation he believes may be at the heart of ME/CFS.