Old Drug Points To a New Way To Knock the Epstein-Barr Virus Down
A recent study suggested that Epstein-Barr reactivation might be present in substantial number of people with ME/CFS. Anti-herpesvirus drug protocols in ME/CFS, however, tend to last very long and aren't always successful. The same drugs have been used for decades. That, however, could be changing, though.Some studies remind us to always be ready for surprises - to not think that we know so much. The body is always throwing us curveballs and it turns out that sometimes drug companies can as well. The spironolactone saga in EBV reminds us that important answers to ME/CFS and other diseases might not need to come from some sophisticated R&D drug program but might literally, right now, be found down the aisles of a pharmacy. Sankar Swaminathan MD, Chief of the Division of Infectious Diseases at the University of Utah, has been publishing on Epstein-Barr virus for almost 20 years. Besides infectious mononucleosis - a common trigger for ME/CFS - EBV has been associated with autoimmune diseases and a host of cancers. Four years ago, Swaminathan and colleagues went on a search to find a drug not to kill EBV - the bug is too firmly embedded in our cells to hope for that - but to stop it from reactivating. It's when EBV awakens from its latent state and begins reactivating that it becomes the most dangerous. If Swaminathan could stop EBV from doing that he would have achieved a momentous goal.He had an important clue. He knew that EBV (and other herpesviruses) produced a protein called SM that played a critical role in the early stages of EBV reactivation. He also knew that current slate of herpesvirus drugs left SM untouched - suggesting the protein presented a new possibility for a new herpesvirus drug.
The Study
Verma D, Thompson J, Swaminathan S. Spironolactone blocks Epstein-Barr virus production by inhibiting EBV SM protein function. Proc Natl Acad Sci U S A. 2016;113(13):3609-3614. doi:10.1073/pnas.1523686113
“It’s remarkable that a drug we have used safely in the clinic for over 50 years is also an effective EBV inhibitor. It goes to show how basic research can reveal things we would never have found otherwise” Swaminathan
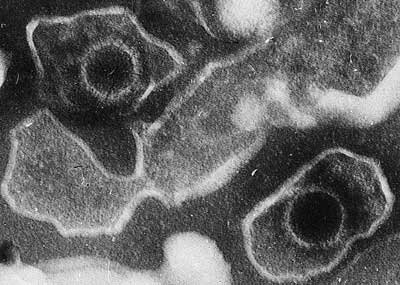
His team found a way to target the protein, and then created an assay that allowed them to screen compounds for antiviral activity. Then came the surprise - spironolactone - a 50 year old drug knocked EBV down. The drug not only stopped EBV from forming the capsid or top layer of EBV that it needs to replicate, but it also blocked the expression of genes the virus used to replicate as well. Spironolactone, though, has never been known as a antiviral. Far from it - it's a mineralocorticoid receptor antagonist used to treat kidney disease, heart failure and edema. The researchers found that its mineralocorticoid antagonist properties weren't suppressing EBV - something else was. Although, the researchers were unsure just how it was doing it, it was clear the drug doing something to EBV that no other drug had done. It had the potential to open a new era of more effective herpesvirus treatments. Spironolactone, itself wasn't the answer. While it's been used for decades it can have significant side-effects. Besides some potentially toxic effects, it also increases the secretion of salts - something that salt craving ME/CFS patients might not find so beneficial.The authors suggested that spirolactone's most important role lay not in the drug itself, but in its ability to pointing to how produce more effective herpesvirus drugs. Noting that the current basket of anti-herpesvirus drugs suffers from problems with side effects and increasing rates of drug resistance, they suggested spirolactone be used "as the template for development of antiherpesvirus drugs".
“We think there is great potential to modify this molecule so that it can work as an antiviral without having undesired side effects,” Swaminathan.
First, though, they would have to find out how Spironolactone was doing what it was doing.
Mystery Solved - and the Hunt for a Better Anti-Herpesvirus Drug Begins
Dinesh Verma1, Trenton Mel Church1, Sankar Swaminathan23Epstein-Barr Virus Co-Opts TFIIH Component XPB to Specifically Activate Essential Viral Lytic Promoters Proc Natl Acad Sci U S A. 2020 Jun 9;117(23):13044-13055. doi: 10.1073/pnas.2000625117. Epub 2020 May 20.
"These findings pave the way for development of antiherpesvirus drugs with new mechanisms of action" Verma et. Al.
Four years later - and at about the same time that an ME/CFS study found direct evidence of EBV reactivation in about a quarter of patients - the mystery of how a kidney drug came to beat back EBV was solved. Spironolactone, it turns out, stops or inhibits the transcriptions of 15 genes the virus needs to replicate. The researchers knew that SM - the protein which had lead to the discovery of spironolactone - enhances the activation of those genes. What they didn't know is that the SM protein does that by ferrying another protein called XPB to EBV's DNA, at which point XPB turns on the genes that begin EBV's replication process. XPB, then, provided a new, earlier, possibly more effective target for shutting down EBV. The University of Utah researchers are now trying to find new drugs that target XPB with the goal of keeping EBV and other herpesviruses in their latent states. Spironolactone, then, didn't turn out to be the EBV inhibitor the medical world is looking for. The 50 year old kidney drug did, however, provided the clue they needed to start developing a new generation of more effective anti-herpesvirus drug. The Spironolactone saga shows that answers to medical issues can come from unexpected places - including old, old drugs - that no one would think to explore.Novel assays - like the one developed by the University of Utah team - and new data mining techniques will undoubtedly provide surprising new insights in the years to come. Some answers to ME/CFS and other diseases could be in plain sight - if only we can see them.